March 2022: The GenOMICC study has identified 16 new genes that might explain why some people progress to becoming critically ill with Covid-19, whilst others experience only mild illness or no symptoms at all.
Examining the whole genome sequence for all participants in the study allowed us to create a precise map and identify genetic variation linked to severity of Covid-19. We found key differences in 16 genes from critically ill patients when compared with the DNA of the other groups.
We also confirmed the involvement of seven other genetic variations already associated with severe Covid-19 discovered in our earlier work.
Our latest discoveries are reported in Nature. Here we present our findings, the discovery and validation of 23 genes and susceptibility to critical Covid-19 by comparing 7,491 critically ill patients from 224 intensive care units, with 48,400 controls (those not affected or with mild symptoms).
These genetic associations suggest biological processes play a role in how our immune response can influence progression to serious illness, including causing inflammatory lung injury seen in severely ill Covid-19 patients. We know that the activity of our genes can be altered by increasing the amount of a particular molecule or signal, so understanding the genetic associations of critical illness is key to being able to identify new treatments.
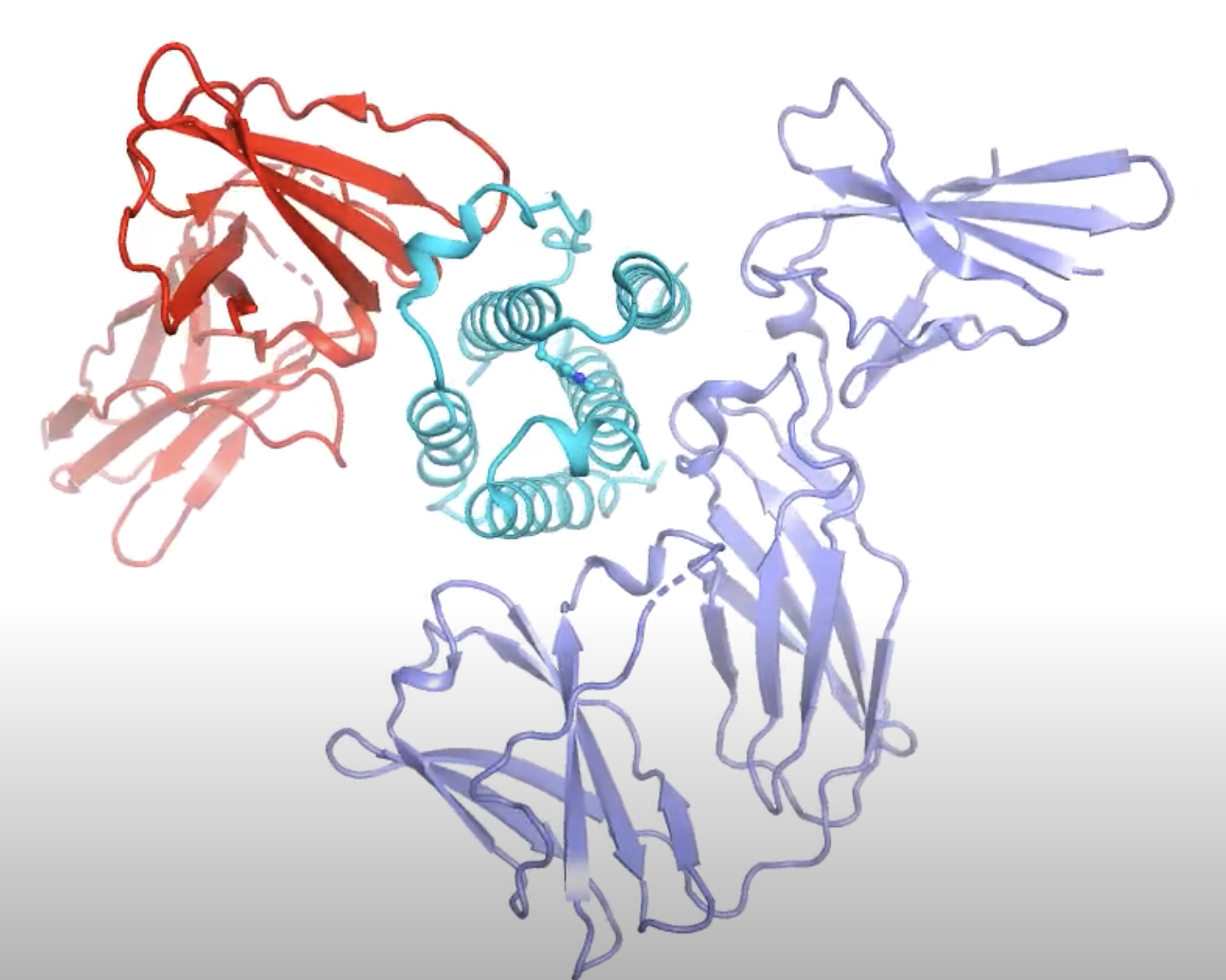
For example, the findings included how a single gene variant that disrupts a key messenger molecule in immune system signaling – called interferon alpha-10 – was enough to increase a patient’s risk of severe disease. This highlights the gene’s key role in the immune system and suggests that treating patients with interferon – proteins released by immune cells to defend against viruses – may help manage disease in the early stages.
Therefore, the identification of specific genetic targets provides signposts for future efforts in finding potential new treatments with pinpoint accuracy. However, this is only part of the solution. Where appropriate, large scale randomised clinical trials are needed so we can find out which treatments work and translate our findings into clinical practice.
Professor Kenneth Baillie, the project’s chief investigator and a Consultant in Critical Care Medicine at University of Edinburgh, said:
“Our latest findings point to specific molecular targets in critical Covid-19. These results explain why some people develop life-threatening Covid-19, while others get no symptoms at all. But more importantly, this gives us a deep understanding of the process of disease and is a big step forward in finding more effective treatments. It is now true to say that we understand the mechanisms of Covid better than the other syndromes we treat in intensive care in normal times – sepsis, flu, and other forms of critical illness. Covid-19 is showing us the way to tackle those problems in the future.”